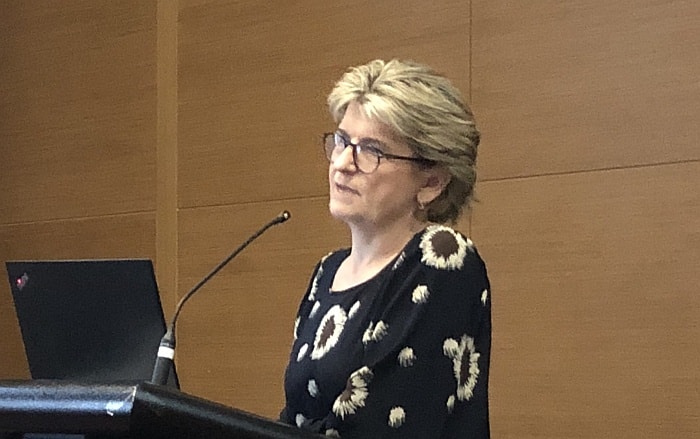
Director Supportive and Palliative Medicine for Western Sydney LHD Dr Sally Greenaway spoke at the Palliative Care NSW Professional Education Day Forum about ‘what matters most’ in policy challenges facing palliative care.
She highlighted 3 themes currently influencing policy development: (1) ensuring that everyone has access to palliative care, (2) the aspirational goal that ‘everyone should be able to die at home’ and (3) advanced care planning as a universal goal.
(1) In ensuring the availability of supportive and palliative care to all she highlighted the relational complexities within end of life care and encouraged policy makers and funding bodies to take into account the effort and value of building relationships:
“Our work is not just about the physical care and the team, it’s about the relationship that exists between the person and their family and the care workers. If that is not there then the care is incredibly hard to give…and the metrics that we use in our work don’t really reflect that.”
Sally spoke about the danger of specialist supportive and palliative care becoming too siloed at the risk of deskilling and alienating their colleagues in other specialty areas and undermine the therapeutic alliance that they form with their patients at end of life. This is particularly significant for patients who move between primary, intermediate and complex care and for whom care coordination is more critical.
“We need to be accessible to everybody and allow everybody to own end of life care. We know where the therapeutic alliance is not honoured and built into the care model then trust gets damaged and people feel abandoned and they are much less likely to organise themselves the way they want to. So we really need to be able to support our colleagues in giving good care and we, as palliative care specialist worker, need to remember that it is not just us who do this.”
Maintaining holistic care, therapeutic alliance and relationship within the constraints of the existing policy and funding settings are significant challenges for palliative care practice going into the future.
(2) Sally also highlighted the emerging narrative in end of life care encapsulated by ‘everyone wants to die at home’ and cautioned against any policy shifts that might compromise the skills, resources and facilities within specialist palliative care.
Pointing to the resourcing challenges experienced by community mental health services in the 80s and 90s, she urged policy makers to consider the real cost of at-home service delivery at end of life, so that the proper allocation of resources follow the shift of policy towards care at home.
“We need to listen to our consumers, our communities, and we need to listen to all our communities. And we need to remember that personal care at the end of life is very messy and physically exhausting and is hugely under-resourced, hence one of the major reasons why people re-enter the acute care sector.”
Although care packages offer support at home, a long wait for a care package means that the person and their carer might not get support before the time of death.
She highlighted the value of the compassionate communities approach and the bottom-up support offered within the community through networks of support, but noted that it also requires top-down engagement with the corporate and government sector for example to improve mechanisms to protect income and offer debt relief for carers.
“Debt moratoriums, donating sick leave to others…there are many ways to support people to die at home but it’s not going to come with small pockets of money, it has to be a whole of society effort.”
(3) Sally also discussed advance care planning and the emphasis on encouraging universal uptake of written advance care directives, particularly over the last 15 years.
She urged us to think more deeply about how we honour the patient’s wishes and what the patient wants, urging practitioners not to simply embrace patient autonomy as a basis to justify treatment.
“The number of patients we see who have had health care (intervention) that wasn’t beneficial, that was never going to be beneficial but was what the patient wanted…to deliver non beneficial care is in fact not ethical.”
Sally also cautioned that a singular focus on the conventional advance care plan approach may serve to minimise the relational complexities embedded in diverse cultures such as those found across western Sydney, in a way that might further marginalise those groups. She identified research highlighting that people who were less likely to identify with dominant cultural groups were much less likely to embrace advance care planning processes, less likely to have an advance care directive and are more likely to find the advance care process intrusive and even destructive to the relationship between the healthcare team the patient and the family.
She noted that for many people the advance care directive aligns with the dominant cultural values around patient autonomy:
So how can practitioners best fulfil their duty of care toward the patient?
“One of the things we do is to ask the patient ‘how much information do you want and how do you like to make decisions? Do you like to know everything, or do you say ‘you tell me what I want to know and just leave it to my daughter or my son or my father or whatever’. Within that conversation the patient is given the right and the freedom to let us know that their autonomy about decision making has been devolved (or not).”
Dr Sally Greenaway was speaking at the Palliative Care NSW Professional Education Day Forum 2018 held at Rooty Hill on the 25th of May, as part of National Palliative Care Week and the theme ‘What Matters Most’.
Pic: Dr Sally Greenaway speaking at the Professional Education Day Forum